
The most common degenerative-dystrophic disease of the spine is osteochondrosis. Its peculiarity is that in the initial stages it does not manifest itself in any way, so many patients turn to the doctor when the processes of tissue destruction have already gone far. But even in this case the diagnosis is not made immediately, but after a series of laboratory and instrumental tests. It is very important to correctly diagnose osteochondrosis, because the earlier treatment is started, the greater the chance of preventing complications. It is for this reason that it is necessary to identify the symptoms of osteochondrosis in time and consult a doctor.
Causes and mechanisms of development
Osteochondrosis begins with destructive processes in the intervertebral discs. They gradually dry out and decrease in volume. This leads to the fact that the disks can no longer perform their functions correctly. They can collapse and then a hernia develops. But very often this condition leads to the development of osteochondrosis.
After all, the intervertebral disc protects the vertebrae from destruction, serves as a shock absorber during various movements and holds the vertebrae in the correct position. When its volume decreases, the vertebrae shift. The instability of a segment of the spine leads to the formation of osteophytes, bony growths that hold the vertebrae apart. Failure to do so may result in pinching of the nerve roots and compression of the blood vessels. All these processes cause the presence of many different signs of osteochondrosis, which is why it is so difficult to diagnose it in time. But if we know why this condition develops, people at risk can be more careful.
Osteochondrosis is usually caused by the following reasons:
- congenital disorders in the development of the spine or connective tissue defects;
- injuries or constant overload, heavy physical work;
- bad posture, flat feet, uncomfortable shoes;
- staying in an uncomfortable position for a long time, sedentary lifestyle;
- obesity, poor diet, excess weight;
- exposure to chemicals, for example, bad habits, taking certain medications;
- frequent stress;
- natural processes that occur during the aging of the body;
- constant vibrating effect on the spine.
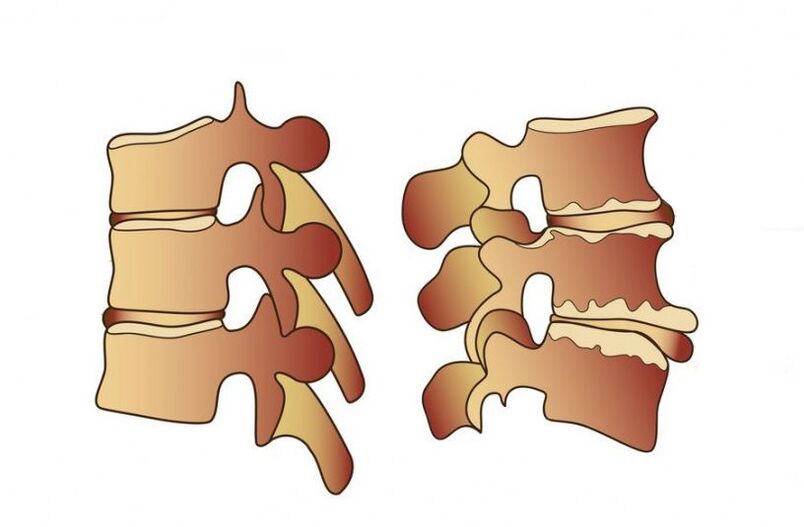
Osteochondrosis develops after a decrease in the height of the intervertebral disc, after which the vertebrae themselves begin to collapse
Therefore, you need to carefully monitor your health to consult a doctor at the first symptoms. This is especially important for athletes, loaders, drivers, gymnasts, women, who often worry about their loved ones and experience stress because of this.
Symptoms
Signs of osteochondrosis depend on the stage of the disease and which part of the spine is affected by degenerative processes. Very often at first the patient does not even feel back pain, only a slight stiffness in the morning. In the process of destruction of the intervertebral disc due to displacement of the vertebrae, the nerve roots are pinched and pain occurs. Depending on the localization of the disease, they can appear not only in the back area. The pain often radiates to the shoulder blade, chest, arm, or leg, and headaches may occur.
A feature of osteochondrosis in the early stages is also that the pain intensifies with physical activity and disappears after rest. Even after adopting a comfortable body position, the patient feels better. Painful sensations worsen after hypothermia, stress, prolonged stay in a static position, for example, when working at a computer or while sleeping on an uncomfortable bed. Very often, with osteochondrosis, stiffness in movements, muscle weakness and constant fatigue are observed. The patient tries to assume a comfortable position in which he feels less pain.

The main sign of lumbar osteochondrosis is pain and stiffness in movements.
Symptoms of lumbar osteochondrosis
The most common site of degenerative-dystrophic processes is the lumbar spine. It can withstand the heaviest loads not only when moving, but also when a person sits in the same position for a long time. Due to the sedentary lifestyle of modern people, the muscle corset here is weak, so any overload can lead to destruction of the discs or displacement of the vertebrae.
In addition to general pain and stiffness, there are special symptoms of spinal osteochondrosis in the lumbar region. If the following signs appear from time to time, you need to make an appointment with a neurologist:
- the lower limbs become numb;
- skin sensitivity is impaired, paresis may develop;
- pain is felt in the pelvic organs, their functioning is disrupted;
- the patient cannot turn or bend, pain is felt even when sitting.
Symptoms of cervical osteochondrosis
It is especially important to know what symptoms the patient with cervical osteochondrosis experiences. After all, sometimes neck pain is not even felt, and other symptoms are similar to vascular disorders that a person is trying to treat with medications. If the destructive processes in the cervical spine are not stopped, this can lead to disruption of the blood supply to the brain and even complete paralysis of the body.
Therefore, it is very important to pay attention to the following signs in time:
- headache that cannot be relieved with conventional analgesics;
- dizziness occurs when you turn your head;
- you may feel pain in the shoulders, back of the head, arms;
- vision deteriorates, colored spots or spots are visible before the eyes;
- there is hearing loss, tinnitus;
- the tongue and fingers become numb;
- coordination of movements is compromised.

With cervical osteochondrosis, headaches and tinnitus are often observed
Symptoms of thoracic osteochondrosis
Signs of osteochondrosis in the thoracic region are easily confused with diseases of internal organs. And although the main symptom is back pain, it has its own characteristics. Patients describe this sensation as if the chest was being squeezed by a hoop. The pain intensifies during inhalation and exhalation, so many attribute these sensations to heart pathologies.
With thoracic osteochondrosis, the pain will intensify with hypothermia, raising the arms and even at night. You may experience numbness in your skin, goosebumps, and coldness in your extremities. Disturbances in the functioning of the digestive system often occur.
Diagnostics
To prevent complications of osteochondrosis, it is very important to consult a doctor as soon as the first signs appear. These are stiffness in movements and back pain after exercise. This pathology is treated by a vertebrologist or neurologist. An experienced doctor can make a preliminary diagnosis during the examination and conversation with the patient.
But some symptoms of the disease are very nonspecific and resemble the manifestations of many other pathologies. Therefore, differential diagnosis is very important, which will help to exclude diseases in which vascular and neurological symptoms also develop. It may be angina pectoris, hypertension, peptic ulcer, pyelonephritis. The main difference between osteochondrosis and them is that it has a chronic course and develops slowly, with periodic exacerbations, and the pain most often disappears with rest.
But without special diagnostics it is still difficult to make a correct diagnosis. Most often, instrumental examination methods are used for this: radiography, CT, MRI, ultrasound, myelography and others. Sometimes laboratory tests may also be necessary. They will help identify the presence of an inflammatory process and an increase in calcium concentration in the blood.
The most common diagnostic method in the initial stage of the disease is x-ray.
X-ray
At the initial stage, X-ray diagnostics is needed to confirm the diagnosis. This is the main examination method for osteochondrosis. It is the simplest and most accessible and has the fewest side effects. After determining the location of the pain, photographs of this area of the spine are taken. They are usually performed in two projections: direct and lateral.
If the diagnosis is made correctly, this will be indicated by the following radiological signs: the distance between the vertebrae is reduced, atrophy of the intervertebral discs is observed, osteophytes are visible, there may be destruction of the vertebral tissue or change in the shape of the spine.
Myelography
This is a more complex method, can have side effects and is not suitable for everyone. After all, myelography is based on the injection of a special contrast liquid into the spinal canal. This could cause an allergic reaction or even spinal cord damage. Next, the spine is x-rayed.
This method allows you to examine the spinal canal and determine where it is damaged by degenerative processes. Furthermore, myelography can determine the presence of intervertebral hernias in the early stage.

MRI is a more informative examination method, so it is used when a differential diagnosis is needed.
Tomography
Diagnosis of osteochondrosis by CT or MRI is made less frequently, since these methods are not yet available everywhere. Therefore, they are used in difficult cases, as well as if it is necessary to differentiate osteochondrosis from other diseases. But with an MRI or CT scan you can examine your spine and surrounding tissues in great detail.
These diagnostic methods allow you to see the state of blood vessels, the presence of hernias, compression of nerve roots and the shape of intervertebral discs. They are necessary for the differential diagnosis of osteochondrosis from osteomyelitis, spinal cord tumors, spondylitis, ankylosing spondylitis and syringomyelia.
Timely identification of the symptoms of osteochondrosis and its correct diagnosis will help to start treatment on time. This will prevent the development of complications, alleviate the patient's condition and reduce the number of exacerbations.

















































