Spinal diseases become younger every year.One of the most common remains osteochondrosis, which has only recently been considered an exclusively age-related disease.If it affects the cervical spine, quite severe pain in the neck, arms and head can occur, significantly reducing the quality of life.This is often accompanied by a number of other disorders and, if left untreated, leads to the formation of intervertebral hernias, large volumes of which require surgical intervention.Therefore, it is important to diagnose cervical osteochondrosis as soon as possible and start treatment according to the situation.

Symptoms of osteochondrosis of the cervical spine
Osteochondrosis of the cervical spine is a disease in which degenerative changes occur in the intervertebral discs.Initially, the discs, which are cartilaginous rings containing gelatinous contents, become dehydrated.This is often the result of a sedentary lifestyle, prolonged computer work, poor posture, neck injuries and a number of other factors.
This leads to a decrease in the resistance of the collagen fibers that form the fibrous ring of the disc.As a result, its thickness gradually decreases, which becomes the main reason for the development of symptoms characteristic of cervical osteochondrosis:
- neck pain of varying degrees of intensity;
- headache, dizziness, loss of consciousness caused by violation of the cervical vertebral arteries passing directly through the vertebrae, that is, the development of vertebral artery syndrome;
- fluctuations in blood pressure levels;
- radicular syndrome, caused by pinching of the spinal roots, which is accompanied by radiation of pain from the neck to the arms, up to the hands and fingers, the head, the shoulders, sensory disturbances in these areas, the appearance of goosebumps, numbness, etc.;
- a decrease in the range of motion of the neck, the appearance or intensification of pain when performing certain movements;
- increased fatigue, decreased performance;
- tinnitus, decreased visual acuity, development of ENT pathologies that are difficult to treat.
There are 7 vertebrae in the cervical spine.Most often, osteochondrosis affects the discs located between the 5th and 6th, as well as the 6th and 7th vertebrae.
In such situations, it is necessary to contact a neurologist who prescribes an MRI.The results of this examination allow you to accurately identify osteochondrosis at any stage, even in the early stage of development, and select treatment.
Development phases
In general, there are 4 stages of development of osteochondrosis:
- Grade 1 – pathological changes are just beginning to appear in the intervertebral disc, so the symptoms are mild and are observed only from time to time.In such situations, the treatment will be as effective and simple as possible.
- 2nd degree: changes in the discs become more pronounced, which leads to the appearance of aching pain in the neck, which occurs and intensifies when performing head movements.
- Grade 3 – pain becomes almost constant and can be complicated by the development of vertebral artery syndrome, as well as the formation of intervertebral protrusion and hernia.
- 4th degree: the disc is so destroyed that the possibility of movement in the affected movement segment of the spine is almost completely excluded.In this case, severe pain is observed, radicular syndrome often develops, and one or both vertebral arteries are pinched, which leads to the appearance of characteristic symptoms.
Treatment of cervical osteochondrosis
Therefore, treatment tactics for cervical osteochondrosis depend on the severity of degenerative changes in the intervertebral discs, the age of the patient and his individual characteristics.Therefore, it is always developed separately for each patient, but is always aimed at solving the following problems:
- elimination of unpleasant symptoms that worsen the patient's quality of life;
- improve the quality of blood circulation in the neck;
- improvement of metabolic processes in the affected area;
- eliminate the causes of degenerative-dystrophic changes in intervertebral discs;
- reducing the risk of developing complications of osteochondrosis, i.e. protrusions, intervertebral hernias, spondylosis, etc.
In general, at each stage of the development of the disease the use of different therapeutic measures is indicated.If in the first stage it will be enough to adapt your lifestyle and engage in physical therapy, then in the second stage a broader impact will be required, additionally including taking a number of medications, conducting manual therapy sessions, using orthopedic devices, etc.
But patients must understand that it is impossible to achieve reverse regression of degenerative-dystrophic changes that have already occurred, especially if stage 2 or higher osteochondrosis is diagnosed.In such situations, treatment will be aimed at improving the patient's well-being and stopping further progression of the disease.Sometimes it is possible to completely correct the situation only in the 1st stage of osteochondrosis, but at this stage of development the pathology is diagnosed very rarely, since patients perceive mild discomfort in the neck only as a sign of fatigue and do not consult a doctor.
In more severe cases, the treatment of osteochondrosis of the cervical spine will be even more complex and long.In any case it is carried out under the supervision of a neurologist with periodic control examinations and adjustment of therapy based on changes in the patient's well-being.
Lifestyle correction
All patients diagnosed with cervical osteochondrosis are advised to make some changes to their lifestyle.In each case, these recommendations vary depending on the characteristics of the person's professional activity and a number of other factors.
The vast majority are advised to increase their level of physical activity and take a break from work at least every hour to warm up if this involves sitting.In cases where the patient is actively involved in sports, it is recommended to reduce the load on the cervical spine.Therefore, he will be shown to give up running, jumping sports, weightlifting and wrestling.
Overweight people are also advised to take measures to reduce it and adapt their diet.When osteochondrosis has already occurred, it is important that the diet meets the daily needs of the body as fully as possible.Therefore, it is worth giving up fast food and semi-finished products and bringing the diet closer to a rational one.This means that it is worth creating a menu so that half of the diet consists of fruits and vegetables, and also contains a sufficient amount of protein.
Pharmacological treatment of cervical osteochondrosis
Drug therapy is primarily aimed at eliminating the unpleasant symptoms of osteochondrosis of the cervical spine.As a rule, it is complex and involves the use of drugs from several groups, each of which solves specific problems.Therefore, it is also developed separately for each patient.
NSAIDs
Nonsteroidal anti-inflammatory drugs or NSAIDs are a large group of drugs that have not only anti-inflammatory but also analgesic properties.They are available in various dosage forms, including tablets, capsules, ointments, gels and creams, as well as solutions for intramuscular administration.NSAIDs should be used only on demand, that is, when severe neck pain occurs.
For severe pain, NSAIDs may be administered intramuscularly.
The disadvantage of oral drugs from the NSAID group is their irritating effect on the mucosa of the stomach and duodenum.This can provoke a worsening of the course of diseases of these organs, in particular gastritis and peptic ulcer.To reduce such risks, proton pump inhibitors are prescribed in combination with them.
There are drugs that have a more gentle effect on the gastrointestinal tract, thanks to which they are widely prescribed to relieve pain and inflammation in osteochondrosis.In addition, more advanced drugs have already been developed, characterized by a selective effect, which are also often prescribed for osteochondrosis, but they are more expensive and are not available to all patients.
Corticosteroids and injections (blocks)
Corticosteroids are hormonal drugs prescribed to patients with severe inflammatory processes.They can cause a number of undesirable consequences with long-term use, so they are prescribed in short courses in the most difficult cases.As a rule, the use of injectable solutions is indicated, since with this method of administration these drugs are much easier to tolerate by the body and are less likely to cause side effects.
Corticosteroids are often used in combination with local anesthetics when performing blockades, that is, to quickly relieve very severe pain by introducing the prepared mixture into special places near the passage of the spinal nerves.The procedure requires certain skills and dexterity and therefore can only be performed in medical institutions by specially trained healthcare professionals.Otherwise, the probability of developing unwanted consequences and complications is very high.
It is recommended to perform blocks no more than 4 times a year.
Muscle relaxants
Muscle relaxants are a group of drugs used to eliminate reflex muscle spasms caused by an acute inflammatory process.This often occurs with cervical osteochondrosis and causes severe pain in the neck, which further aggravates the situation.
Vitamins
Since osteochondrosis creates significant prerequisites for compression of the spinal roots, the intake of vitamin complexes containing mainly B vitamins is often indicated. They are directly involved in the transmission of nerve impulses, which is especially important in the development of radicular syndrome.
Chondroprotectors
Chondroprotectors are drugs around which much controversy rages.They are based on substances used by the body to restore damaged cartilaginous tissue, which determines the indications for their use in cervical osteochondrosis.At the same time, however, there is no convincing evidence of their effectiveness in advanced forms of the disease.In the initial stages of osteochondrosis they have a positive effect on the state of the intervertebral discs, which leads to an improvement in the patient's well-being.And in later stages they can only help inhibit the further progression of degenerative changes in the intervertebral discs.
Chondroprotectors are produced in the form of powders for the preparation of solutions, capsules, products for topical use, as well as solutions for intramuscular administration.The greatest positive effect was found by the latter.
Topical products
These are precisely the drugs, available in the form of a gel, cream or ointment, that patients often begin to use when signs of cervical osteochondrosis appear.They have different effects, including anti-inflammatory, analgesic, warming or, conversely, refreshing and local irritating.
These products often contain NSAIDs, so they help reduce pain, but they are especially effective in the early stages of osteochondrosis.Also, the components of such drugs can be menthol, chili pepper extract, snake or bee venom.
Local irritants act on the principle of irritation of the nerve endings of the skin, due to which there is a decrease in the severity of pain and an increase in blood flow to the area of application.But such means are effective only in the initial stages of the development of cervical osteochondrosis.
Prepare to improve microcirculation
Drugs from this group are used to improve the quality of blood circulation, which is especially necessary for vertebral artery syndrome.Numerous drugs have a vasodilatory effect, which improves brain nutrition and helps eliminate tinnitus, headaches and dizziness.But without effectively eliminating the factor that puts pressure on the vertebral artery, such treatment will only provide temporary results.
Physical therapy
Physical therapy is the basis for the treatment of osteochondrosis of the cervical spine.Today, there are many different patented and generally accepted methods of physical therapy for cervical osteochondrosis, but patients should understand that there are no universal exercises.A set of exercises should be selected by a specialist on an individual basis, taking into account not only the stage of development of degenerative-dystrophic changes, but also the age of the patient, the nature of existing concomitant diseases, the presence of radicular syndrome or compression of the vertebral arteries.Therefore, different exercises may be indicated for the same patients with approximately the same changes in the intervertebral discs.
In general, physical therapy has the following goals:
- strengthen the muscles of the neck and upper shoulder girdle;
- activation of blood circulation in the affected area, which will contribute to the restoration of the fibrous rings of the intervertebral discs;
- normalization of muscle tone.
It is necessary to do physical therapy every day.At first, it is best to attend special groups or work individually with a physical therapy instructor.This will allow you to 100% master the technique of performing each proposed exercise so that its implementation brings maximum benefit.The specialist will help you select the optimal load and develop a program for increasing it, taking into account the patient's level of physical development.

In the future, patients will be able to practice physical therapy independently at home.At the same time, it is important to approach it with full responsibility, perform the exercises slowly, without haste and in comfortable conditions.But if pain appears at any time during exercise, you should immediately stop performing the exercise that provoked its appearance and consult your doctor to determine the causes and correct the physical therapy program for cervical osteochondrosis.
When performing physical therapy, it is prohibited to make sudden and strong movements, rotate the head or perform exercises in case of pain.In such situations, there is a high risk of exacerbating existing changes in the disks instead of achieving the expected benefit.
Swimming has a very positive effect on the condition of the spine.This is exactly the kind of sport that places no stress on the discs, but actively engages the back and neck muscles.As a result, the muscle corset is effectively strengthened, serving as a natural support for the spine.Therefore, if possible, patients are advised to visit the pool 2-3 times a week.
Manual therapy for cervical osteochondrosis
Manual therapy is one of the most effective methods of treating cervical osteochondrosis, as it allows you to influence not only the muscles and soft tissues, but also the spine itself.But it is very important to take a responsible approach when choosing a chiropractor, since incorrect or too strong influence can lead to a worsening of the patient's condition and even the development of complications.Such a specialist must not only have a higher medical education and a license to practice manual therapy, but also have in-depth knowledge of the features of anatomy and osteochondrosis and have sufficient experience.
Do not confuse manual therapy and therapeutic massage.The differences between these types of manual therapy are notable, since therapeutic massage involves only the soft tissues, while in manual therapy the doctor also intervenes on the spine.
Therefore, each manual therapy session begins with a caress, which allows you to prepare the skin for more active subsequent effects.In the future, rubbing, kneading and squeezing techniques will be used, which allow you to activate blood flow in the collar, neck and upper back area.As soon as the skin and muscles are sufficiently warmed up and the patient is relaxed, the doctor begins to perform mobilization and manipulation techniques.They involve the implementation of turns with oscillatory movements, pushes in the direction of the most pronounced restriction of movement, which leads to increased mobility of the spine and the elimination of functional blocks.
Therefore, thanks to qualified manual therapy, it is possible:
- normalize the position of the vertebrae, thus eliminating the increased pressure on the intervertebral discs and creating favorable conditions for their restoration;
- eliminate the pain caused by cervical osteochondrosis and its complications;
- bring overly relaxed muscles back to normal tone and relax spasmodic muscles;
- increase neck mobility;
- eliminate pressure on the vertebral arteries and thus normalize blood flow to the brain;
- eliminate compression of the spinal roots and thus normalize the conduction of bioelectric impulses to those innervation organs for which they are responsible, as well as reducing pain.

It is especially worth highlighting the author's method of manual therapy.It involves the use of special patented impact techniques, which allow obtaining a pronounced result already after the 1st session, not only on the part of the neck affected by osteochondrosis, but also on the entire body.As a result, not only do pain and other symptoms of the disease disappear, but the functioning of all organs improves and the immune system is strengthened.The second and subsequent sessions enhance the positive effect and consolidate it, which guarantees that, if other medical recommendations are followed, the remission period will last as long as possible.
Self-massage
To improve their well-being, patients can periodically perform neck self-massage to relieve feelings of tiredness and reduce pain.To do this, sit in a comfortable position and try to relax your neck muscles.Then perform stroking movements with your palms, gradually moving to circular rubbing, capturing the shoulder area.All movements are performed by the spine without sudden and strong pressure.In this case you can use local anti-inflammatory drugs recommended by your doctor.
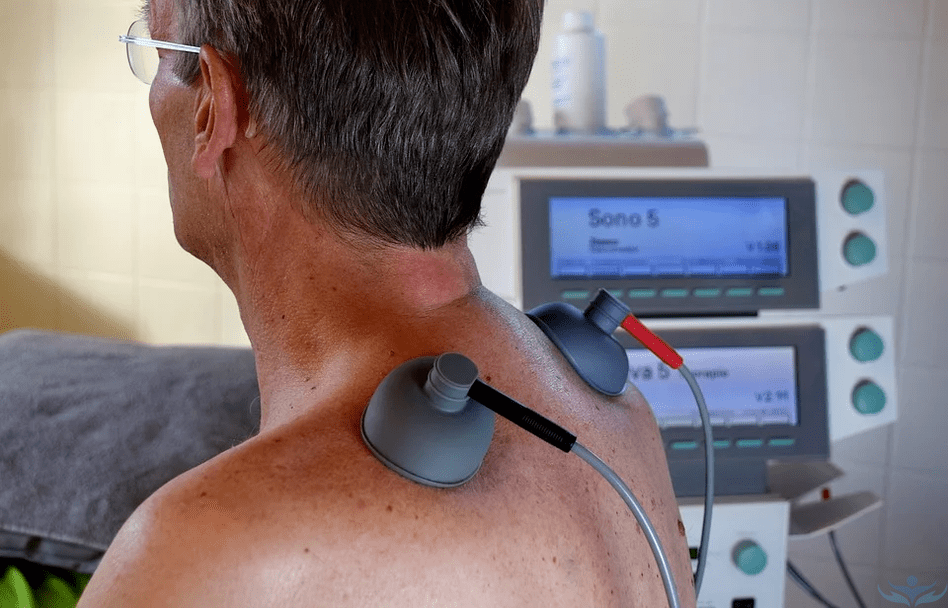
Physiotherapy treatment
Physiotherapy is indicated outside of the acute inflammatory process.It allows you to consolidate the treatment results obtained and further improve the patient's condition.As a rule, a course of 10-15 procedures is prescribed, selected separately for each patient.Could be:
- Electrophoresis: involves the use of electric current to ensure deeper penetration of the indicated drugs.
- Magnetotherapy – helps activate blood circulation in the area of influence and stimulates the course of metabolic processes.Furthermore, magnetotherapy sessions have an analgesic effect and help eliminate swelling.
- Laser therapy has an anti-inflammatory and vasodilatory effect, which leads to a decrease in the severity of pain.
- Ultrasound therapy is a physiotherapy method based on the positive effect of ultrasound waves on the body.They help reduce the sensitivity of nerve endings and also have an anti-inflammatory and analgesic effect.
- Diadynamic currents – procedures lead to a reduction in pain, improve tissue nutrition, have a positive effect on muscles and help eliminate inflammation.
Traction therapy
When the vertebrae join together due to flattening of the intervertebral discs, traction therapy using a Glisson loop is indicated.The essence of the method is to apply a precisely adjusted tensile load to the cervical spine using a special device that fixes the head and has a load on the opposite side.Such procedures help to increase the distance between the vertebrae, which leads to a decrease in pressure on the discs and creates favorable conditions for their recovery.But such therapy can only be prescribed by a doctor.

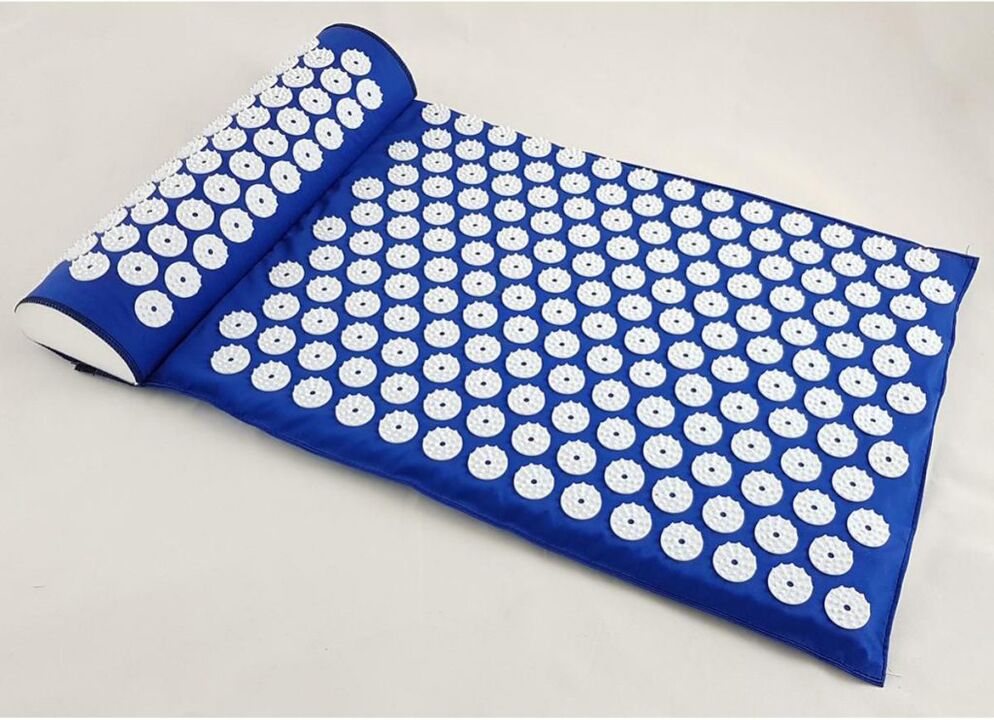
Needle applicator
The iplicator is a simple and economical means of practicing foot reflexology on the neck area.This could be a plate with spikes to place under the neck or a similar device, but in the shape of a roller.Due to the tingling of the spines, the skin receptors are irritated, which leads to more active blood flow in the affected area.
Some patients note a decrease in neck pain after using the applicator, as well as increased performance, improved sleep quality, and restoration of neck mobility.But if you have skin lesions in the affected area or vascular disease, you should not use a needle applicator.
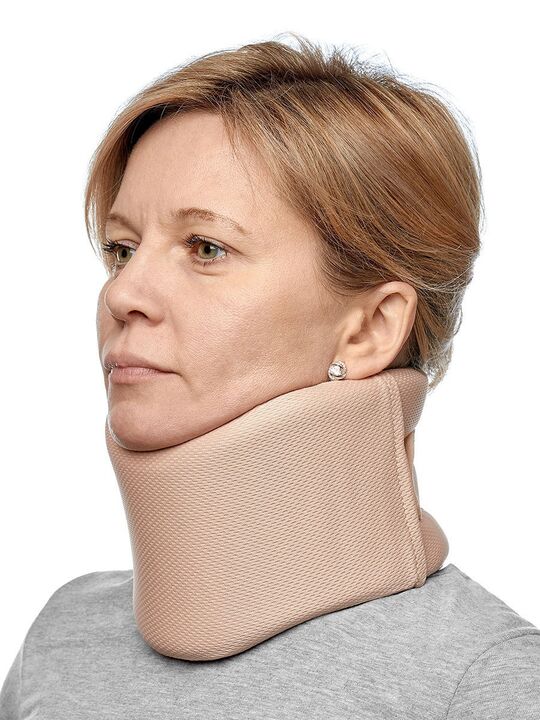
Orthopedic devices
To reduce the load on the cervical spine, it is recommended to change the mattress and pillow to orthopedic ones, since sleeping on an uncomfortable pillow causes additional compression of the vertebral arteries and nerve trunks during sleep.Orthopedic products are free from this drawback and guarantee the maintenance of the physiologically correct position of the spine along its entire length and therefore reduce the speed of progression of existing osteochondrosis.
But it is important to choose the right pillow and mattress so that they match the patient's individual characteristics and contain adequate padding.Thanks to them it will also be possible to improve the quality of sleep and wake up in the morning cheerful and rested.
Additionally, some patients are advised to wear a Shants collar.It is a removable orthopedic device that allows you to fix the neck and significantly reduce the load on the cervical spine, for example when working at the computer or after suffering an injury.The collar is worn before the expected load on the neck, but must be removed during sleep and rest.They differ in design, height, degree of fixation, so only the attending physician can choose the optimal one.
Therefore, the treatment of cervical osteochondrosis can be quite long and complex.You should be prepared for this, because there is no other way to stop the development of changes in the intervertebral discs, avoid the development of complications and the need for surgical intervention.But in most cases, patients' condition improves within the first few weeks of treatment.At the same time, it is important not to self-medicate, but to contact a neurologist, since only a qualified specialist will be able to determine the degree of osteochondrosis and select the most appropriate treatment for the disease for a particular patient.

















































