The hand is the most complex region of the upper limb in its structure. It consists of many bones, closely grouped. The bones are connected through 30 different joints: interphalangeal, metacarpophalangeal, carpometacarpal and radiocarpal.
According to statistics, the hands are injured much more often than any other part of the body. Various injuries represent, according to various sources, from 30 to 50% of the total number of injuries of the musculoskeletal system and do not tend to decrease.
Therefore, of all the causes of pain in the fingers, the main one is trauma. In second place in terms of prevalence are connective tissue diseases - rheumatoid arthritis, systemic scleroderma and lupus erythematosus, psoriasis. Much less often, pain in the joints of the fingers is due to a violation of metabolic processes in gout, arthrosis.
Symptoms
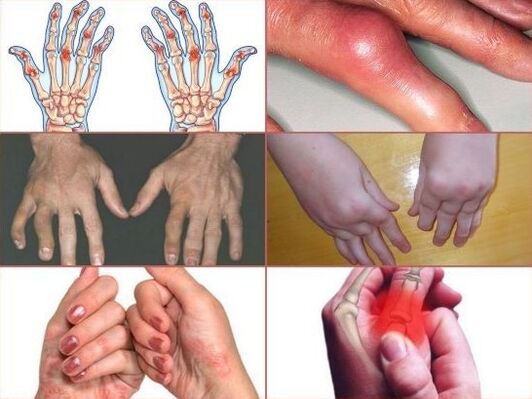
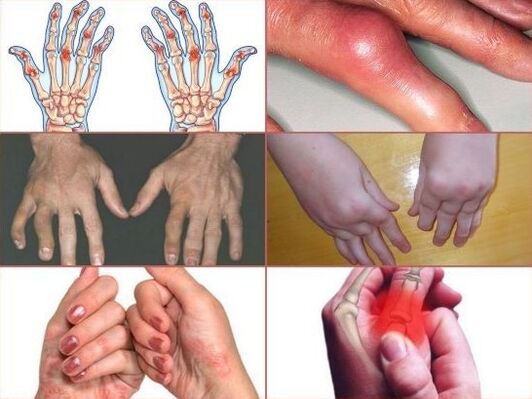
Signs of non-traumatic injuries that may indicate the presence of joint pathology are the following:
- pain syndrome, which is permanent or wavy;
- pain when pressing and bending the fingers;
- swelling and redness of the skin on the joints;
- stiffness, stiffness during movements;
- deterioration of fine motor skills;
- creaks, creaks and crackles when flexing the fingers;
- the formation of subcutaneous nodules, painless to the touch;
- thickening of the skin at the folds;
- change in the configuration of the joints;
- increase in body temperature.
Rheumatoid arthritis
Rheumatoid arthritis most often affects the fingers and the right and left hands at the same time. This systemic disease is characterized by a malfunction of the immune system, in which T lymphocytes begin attacking their own cells. The cells of the synovial membrane that line the joint capsule from the inside actively produce rheumatoid factors: pathological antibodies are protective protein molecules.
Subsequently, rheumatoid factors enter the bloodstream and bind to normal antibodies. As a result, immune complexes are formed that are deposited on blood vessels and tissues. They are absorbed by the cells of the immune system: neutrophils and phagocytes, releasing substances that damage the surrounding structures.
It is known that this is how inflammation develops in rheumatoid arthritis. However, the scientists were unable to determine the cause of this process. According to the latest research in this area, the culprits of connective tissue damage are cytokines, which signal immune cells. Japanese experts came to the conclusion that the study of this cellular type will help to find an effective method of treatment.
With rheumatoid arthritis, any finger can hurt: index, middle, ring or little finger, but the injury will always be bilateral. If one or more fingers of the left hand get sick, the very fingers of the right hand begin to hurt almost immediately.
The phalanges in the area of the joints swell and redden, due to the accumulation of fluid, do not bend well, especially in the morning. Morning stiffness can last up to 1 hour. Over time, the progression of arthritis leads to the replacement of smooth cartilage tissue with a fibrous structure, which disrupts the free movement of the bones in the joint.
Gradually, the joints are deformed, due to a change in the position of the joint elements, the pain intensifies. With a long course of the disease, small painless formations appear near the joints on the back of the hand - rheumatoid nodules.
Psoriatic arthritis
Symptoms of this disease can resemble rheumatoid arthritis and occur against the background of a dermatological pathology - psoriasis. In the vast majority of cases, rashes appear first, and after a while the joints of the fingers ache.
Simultaneous manifestation of skin and joint lesions is also possible; in 20 out of a hundred patients, the joints begin to hurt earlier. Why psoriasis occurs is unknown. Presumably, it can be caused by a genetic predisposition, a malfunction of the immune system and infections. The average age of the patients is 40 years.
Psoriatic arthritis can start, like rheumatoid arthritis, with general weakness and malaise, or it can manifest itself with unexpectedly sharp painful sensations. Not only the fingers can be affected, but also the small joints of the feet, knees and shoulders. Involvement in the pathological process can be both one-sided and symmetrical.
Pain syndrome is most pronounced at night and at rest. In the morning there is stiffness, during the day and with movements the pain subsides. Most often, there is a lesion on one side - to the left or to the right, and, as a rule, it hurts not one, but 2-4 joints (oligo-arthritis).
After a long rest, the fingers become very swollen and become like sausages, the tendons of the flexor muscles become inflamed, the skin over the joints acquires a bluish-purple tinge. The following symptoms indicate the presence of psoriasis and psoriatic arthritis:
- red or pink scaly patches on the head, elbows, knees and thighs: they can be single or cover a large area of the skin;
- characteristic dimples on the skin of the hands, similar to smallpox, pigmentation on the fingers or toes;
- psoriatic plaques are hyperemic, edematous and can itch;
- joint pain is permanent and does not go away during the day;
- the mobility and functionality of the hand are significantly reduced.
The arthropathic form of psoriasis is one of the most serious. Deformation of the joints is usually not observed, but if this occurs, fusion of the articular surfaces of the bones (ankylosis) is not excluded.
The danger of this disease is that the large joints and the spine are gradually involved in the pathological process. Bone osteoporosis develops, joints are destroyed, so psoriatic arthritis often leads to disability.
Osteoarthritis
With osteoarthritis, the process of forming the cartilage tissue covering the joint surfaces of the bones is disrupted. This is facilitated by both external and internal factors: injuries, high physical activity, hereditary predisposition and metabolic disorders.
Depending on the cause, osteoarthritis can be primary and secondary, developing against the background of an endocrine or metabolic disease. Most often, osteoarthritis affects the large joints of the lower extremities - knee, hip and ankle - because they bear the main load when walking and standing. The upper limbs are affected much less frequently.
When the fingers ache as a result of prolonged physical exertion and after rest the pain disappears, the development of arthrosis is not excluded.
Over time, other symptoms appear:
- increased pain when clenching a fist or straining the fingers;
- an increase in the size of the diseased joint;
- morning stiffness, requiring the "development" of the fingers for 10-15 minutes or more;
- characteristic crackle when bending the fingers.
Osteoarthritis develops slowly and may not cause much concern for several years or even decades. However, in some cases, there is a rapid increase in symptoms and a sharp deterioration in the condition. If at first the pain occurs only during exertion, later it does not disappear even after rest.
Due to the marginal outgrowths of the bones that form the joints, characteristic pineal formations appear. Closer to the palm, in the joints of the proximal phalanx, Bouchard's nodules are formed. Next to the distal interphalangeal joints, located near the nails, are Heberden's nodules.
Stenosing ligamentitis
Stenosing ligamentitis affects the ligamentous tendon apparatus of the hand and occurs when one of the fingers is locked in a flexion or extension position. The pathological process is caused by overload or excessive pressure on the ligamentous area, so the disease occurs among people engaged in manual work - bricklayers, welders, seamstresses and kitchen workers. In children, stenosing ligamentitis is extremely rare and affects only the thumb.
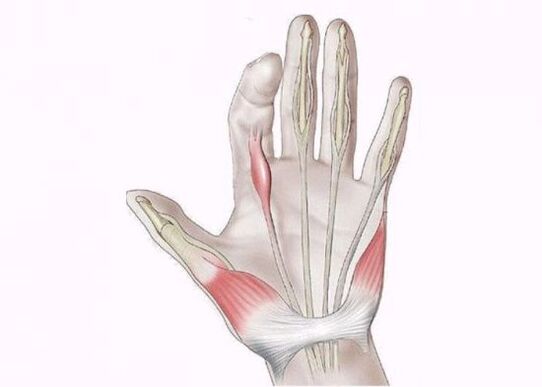
The main symptom of the disease is the "jumping" of the finger during extension, accompanied by a click. In the future, the "click" disappears and the finger remains motionless, turning into a flexion or contracture of the extensors.
In the early stages, there is pain when pressing on the palm at the base of the finger and difficulty in flexion / extension, especially pronounced in the morning. With a long course of ligamentitis, you can move your finger only with the help of the other hand, and after the "snap" there is a pain that spreads not only to the palm, but also to the forearm.
Which doctor to contact
For finger pain, you can first contact a therapist who, if necessary, will refer you to a narrow specialist: a traumatologist, rheumatologist, hematologist, neurologist or surgeon. Clinical, radiotherapy and laboratory research methods are used for diagnosis.
To find out the cause of the pain, a childbirth (history collection) and physical examination are performed, after which an x-ray or tomography, blood and urine tests are prescribed.
Treatment
How to be treated and what to do next will depend on the exam results. Task number 1 is to relieve pain and inflammation - drugs from the NSAID group are prescribed for this - non-steroidal anti-inflammatory drugs. Currently, more and more often used means of the new generation, NSAIDs of selective action.
Selective NSAIDs act selectively and have less toxic effects on the body, they can be taken for a long time. If the pain syndrome is moderate or mild, then topical agents are used - anti-inflammatory ointments and gels.
The treatment of rheumatoid arthritis includes basic and biological products, steroid hormones. These drugs suppress the immune system, thereby reducing the intensity of the inflammatory process.
The same immunosuppressive drugs are prescribed if the joints hurt against the background of psoriatic arthritis. Methods such as plasmapheresis, hemoabsorption and photochemotherapy are used to reduce the activity of the disease, prolong the periods of remission and shorten the duration of drug therapy.
How to treat osteoarthritis of the joints depends on the stage of the disease. In stages 1-2, it is possible to significantly slow down the destruction of cartilage by taking chondroprotectors. Physiotherapy is effective, which enhances the effect of drugs and stimulates recovery processes.
For the treatment of arthrosis can be prescribed:
- magnetotherapy;
- electrophoresis;
- laser;
- ultrasound;
- cryotherapy - exposure to the joints with liquid nitrogen;
- balneotherapy - baths with mineral water;
- Hirudotherapy - during treatment with leeches, substances that promote cartilage regeneration (hirudin, vitamins and hormones) enter the joint.
Therapeutic tactics for stenosing ligamentitis is determined taking into account the stage, the presence of provoking factors and the age of the patient. If the damage to the ligaments is minimal, it is recommended to reduce the load on the hand, if necessary, the hand is fixed with an orthosis or splint. For pain, anti-inflammatory drugs and electrophoresis with hyaluronidase are prescribed.
Treatment of the second stage begins with conservative methods. Lack of effect for several months is an indication for surgery to cut the damaged ligament. In patients with the third stage, conservative therapy is performed very rarely, in most cases, surgical intervention is performed as intended.
Reference: Due to the high risk of relapse, it is very important to change professions if it involves a load on the hands.
Folk remedies
Means prepared according to folk recipes cannot be the main method of treatment, as they are not effective enough. However, as an adjunct therapy, such drugs will help relieve pain and enhance the effect of drugs.

Mix a few bay leaves with juniper needles, add a little butter and massage your hands with the resulting ointment.
At night, you can make a compress of chopped chalk, kefir, fermented cooked milk or boiled oatmeal.
For compresses, green potatoes are used, which must be chopped directly into the peel in a meat grinder or on a grater. Then dip the potato puree in hot water and heat it to 39-40 °. Next, put it in a linen bag and apply it to the sore joints for half an hour. The procedure can be done several times a day.
Paraffin applications relieve pain well, if you put your hands in the melted paraffin for 10 minutes and then hold them in a decoction of herbs for 15-20 minutes. You can not be afraid of burns, as paraffin melts at a temperature not higher than 65 °. To get the effect, 2-3 applications per week are enough.
Compresses with Bischofite help accelerate tissue healing. Thanks to its composition, this natural mineral relieves pain and inflammation, restores joint mobility. Regular use of Bishofit maintains the tone of the muscles and connective tissues.
It is advisable to carry out a compress with Bischofite as follows: warm the joints with a heating pad or keep them in a hot bath, then rub Bischofite, previously diluted with water 1: 1, on the skin of the hands. The rubbing should continue for several minutes, after which a cloth or gauze soaked in the solution is applied to the sore spot. From above, the compress is covered with polyethylene and insulated. Compresses with Bischofite are made at night, in the morning the hands are washed thoroughly with warm water. The procedure is done every other day for three weeks.
Reference: A compress with Bischofite can be applied simultaneously on no more than three joints.
The most important
To prevent or reduce the intensity of pain that has already appeared, it is necessary to keep the brushes warm and not expose them to hypothermia. Work that requires performing the same type of movements is best done intermittently and when using vibrating tools, use gloves and support the working brush with the other hand. When lifting and carrying heavy loads, the weight of the load must be evenly distributed on both limbs. You can also keep your joints healthy with the help of proper nutrition, which must contain foods containing calcium and omega-3 fatty acids.

















































